How Does Gestational Diabetes Impact Pregnancy, Childbirth, And Diet Options?
Whether you are expecting your first child or your fourth, all pregnancies can cause some anxiety. We may go on and on about handling the physical side effects of pregnancy. These are nausea, exhaustion, swollen ankles, as well as hormonal mood swings and anxiety overall. Everything looks even more burdensome once gestational diabetes is identified in the combination.
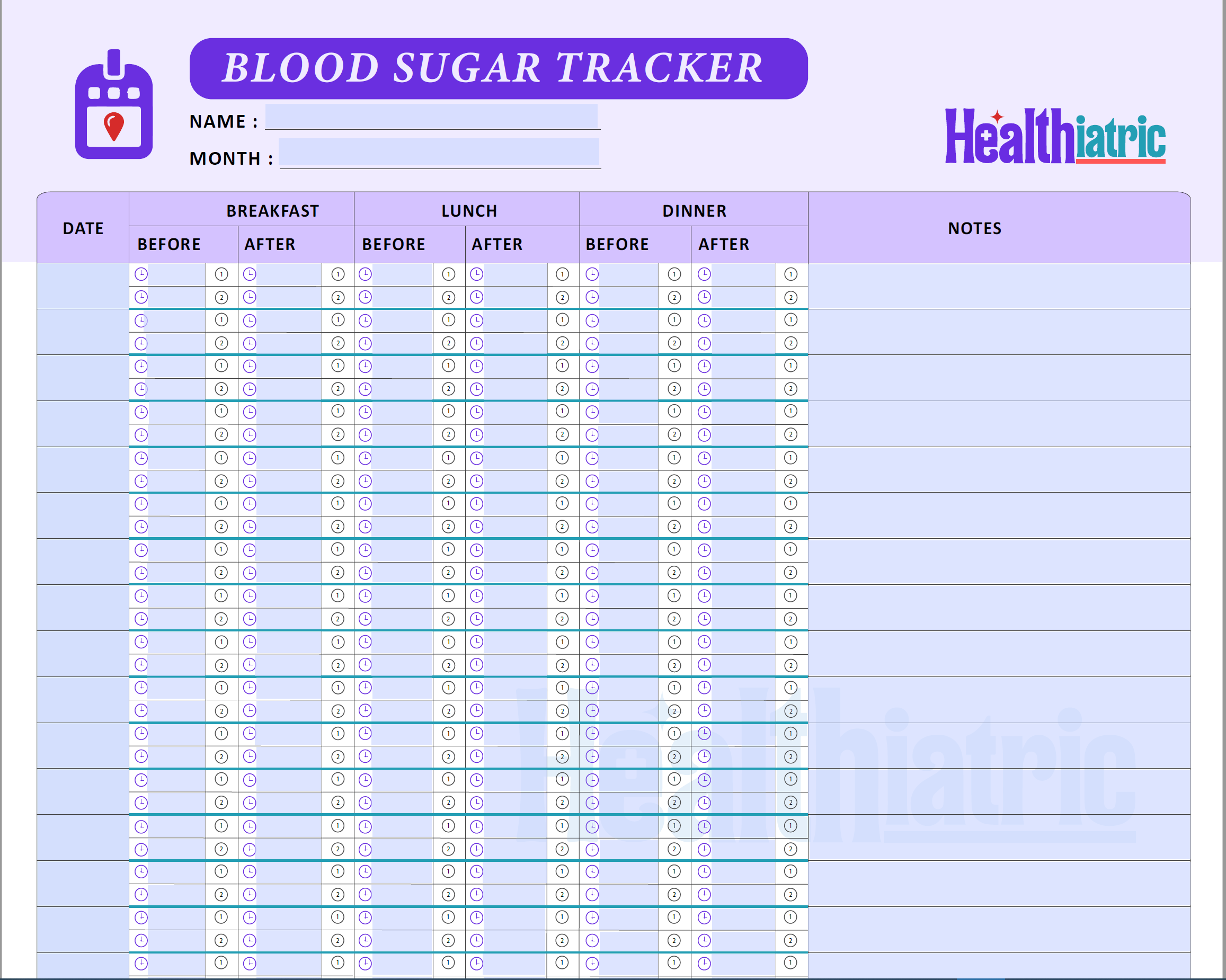
Gestational diabetes demands the monitoring of blood glucose levels even after birth. Here are some associations of gestational diabetes with the birth process and medication intake.
- Gestational diabetes can increase the risk of preterm labor due to complications with the placenta.
- Babies born to mothers with gestational diabetes may have higher birth weights, often called macrosomia.
- Uncontrolled gestational diabetes can result in babies developing low blood sugar (hypoglycemia) shortly after birth.
- Hormonal changes during pregnancy can make cells more resistant to insulin, worsening blood sugar control.
- Gestational diabetes can sometimes affect the baby’s long-term metabolic health, increasing their risk of diabetes later in life.
- Women with gestational diabetes are at higher risk of postpartum depression due to hormonal and physical stressors.
What does Gestational Diabetes Indicate?
It’s a simple diabetes that occurs during conception. One in seven women often suffers from gestational diabetes and it is diagnosed between 24 to 28 weeks of pregnancy. Though gestational diabetes fades away after delivery, most women experience type 2 diabetes and future gestational diabetes as major complications.
What Causes Gestational Diabetes?
Diabetes indicates higher amounts of glucose in the bloodstream. This glucose is the major energy source for the body and comes from carbohydrate foods like starchy vegetables. Our body converts these carbohydrates into glucose, which, in return, enters the bloodstream.
Insulin plays an important role by allowing this glucose to enter body cells and used for energy. During conception, some hormonal changes induced by the placenta impair the functioning of insulin. It exerts a load on the pancreas to secrete more insulin.
If the pancreas cannot produce this extra insulin, it leads to the development of gestational diabetes.
Symptoms of Gestational Diabetes
There are some common signs of gestational diabetes that everyone should understand. Here are some of the major;
- Increased feeling of thirst
- Dry mouth
- Blurred vision
- Lethargy
- Genital itching
- Weight loss
- Frequent urination
Gestational Diabetes and Medication Therapy
Some women are concerned that beginning medication would indicate that they haven’t taken care of their gestational diabetes enough or that it is becoming worse. Using medication does not show failure.
It simply shows that your body requires additional support to maintain blood glucose levels. Also, keep in mind that each woman’s experience with gestational diabetes and its management may vary.
Common Diabetes Supplies
NDSS stands for National Diabetes Services Scheme. It provides accessibility to discounted medications to be used for managing blood sugar levels. Two major products include;
- Blood glucose testing strips at discounted price
- Insulin syringes and pen needles with no cost
You must have to be registered on the national diabetes services scheme to purchase these discounted products.
Intake of Insulin and Hypoglycemia
Blood glucose levels decrease excessively if you are taking insulin to treat gestational diabetes. When these levels fall below 4 mmol/L it is known as hypoglycemia. Though, this is not a commonly occurring condition, but shows the possibility of occurrence somehow.
This state is often caused by multiple conditions, too. For example;
- Missing a meal
- Not having adequate carbohydrates
- Taking too much insulin
- Staying more active than normal
Nausea, lethargy, shivering, perspiration, and dizziness are some hypoglycemia symptoms. Monitor your blood sugar levels if you are using insulin to treat gestational diabetes and experience any of these signs.
Treat the hypoglycemia if it is lower than 4 mmol/L. This treatment of hypoglycemia is suggested to prevent blood sugar levels from falling.
It is advised to take some carbohydrates having better absorptive capacity. Some equivalents of good carbohydrate sources are:
- Glucose gel is equal to 15g carbohydrates
- 6 or 7 normal-sized jelly beans
- 3 teaspoons honey or sugar
- Half-glass fruit juice
- Half a can of a soft drink
After taking any of the sources, wait for around 10 to 15 minutes and then check blood glucose levels. If they are above 4 mmol/L, it means the hypoglycemic state is no longer existing. If your sugar levels remain below this range, then repeat the treatment.
If your next meal is around 20 minutes away, have some additional carbohydrate sources like fruit, a glass of milk, or a cup of yogurt.
There is no evidence that hypoglycemia affects the unborn child. However, it is advised to treat this condition, as it can endanger the safety of the mother.
Diabetes and Birth Process
During conception, your baby and you are under the care of diabetes and pregnancy health providers.
This involves routine blood pressure measurements and ultrasounds to monitor your baby’s development. As necessary, additional blood tests may also be scheduled.
The medical practitioners who are monitoring your pregnancy may advise “inducing” the delivery one or two weeks early if the baby gets too big or if there are any other pregnancy-related issues.
If a premature birth is necessary, labor is typically induced by the administration of a drug that gets the cervix ready for delivery.
C-Section
You run the same probability of requiring a cesarean birth as every pregnant woman. If the baby is very large or if there are additional reproductive complications, such as a lower placenta, transverse appearance, or a previous cesarean delivery, a C-section delivery may occasionally be necessary.
Discussing C-sections with your healthcare providers is a good idea so that you are informed if the situation ever occurs.
Insulin Drips
You may be required to administer insulin intravenously or orally to manage signs of gestational diabetes during labor or a cesarean section. This is more frequent in pregnant women who need therapy with large doses of insulin.
Although it is unusual, some women may also require a glucose drip during delivery.
Post Birth Monitoring of Blood Glucose Levels
A pediatrician, your obstetrician, or a midwife evaluates your kid after birth. For the first 24-48 hours, the heartbeat, respiration, color, and blood glucose levels of infants are closely monitored.
Baby’s levels of blood glucose levels are checked by the nurses through heel pricks. If this appears below 2.6mmol/L, supplemental feedings are suggested for the child.
However, breast milk can be used as an additional feeding source, but after getting approval from the pediatrician.
Medication Advice after Baby Birth
Following the baby’s birth, the medications like insulin or metformin are often stopped. Meanwhile, the doctor’s team suggests monitoring blood glucose levels frequently. If they come up between 4 to 8 mmol/L, they are normal.
Meanwhile, if they fall in the gestational diabetes range, seek further help from medical professionals.
6 to 12 Weeks after Birth
After giving birth, most women don’t have diabetes, however, some still have higher blood sugar levels. To ensure that blood glucose levels have stabilized, an oral glucose tolerance test (OGTT) is crucial.
You are instructed to have this test 6–12 weeks after the birth of your child.
Preferred Food Choices for Gestational Diabetes
When you have gestational diabetes, it’s important to eat a healthy diet that provides you and your unborn child with all the nutrients you need without raising your blood sugar levels excessively.
A healthy gestational diabetes meal plan is something that is recommended for pregnant women with diabetes. It provides health benefits to you as well as every member of your family.
Choose Complex Carbohydrates
It is always advised to choose complex carbohydrate food sources rather than simple carbs. Simple carbs contain more sugar, which is not good for a diabetic patient. Healthy carbohydrate food sources provide essential nutrients, including vitamins, minerals, and fiber, for the mother and the developing child.
Here are some tips for the intake of complex carbohydrates and maintaining blood sugar levels meanwhile.
- Divide carbohydrate servings into three main meals and three snacks throughout the day.
- Don’t take a higher portion of carbohydrate-rich foods at one time. Try to divide the meals into portions. As, eating often but in small portions does not raise glucose levels excessively.
- Never skip any meal. It will help you not eat too much at the next meal.
- Cut off sugary foods like cakes, chocolate, and soft drinks.
Healthy Snacks Options
There are multiple snack options available in the market. It becomes very difficult for a diabetic patient to choose a healthy snack. So, here are some options presented for convenience.
- 1 medium piece of any fresh fruit like a banana or a bowl of fruit salad.
- 1 small glass of fruit smoothie made using banana, mango, berries, and skim milk.
- 1 cup low-fat yogurt without sugar. For example, low-fat Greek style fruit yogurt.
- 1 slice of fruit toast or whole grain bread with margarine or nuts spread.
- 1 handful of dry fruits.
- 3 Dates.
- Plain sweet biscuits like milk, Arrowroot or Milk Coffee.
- Low-fat milk with 1 teaspoon of milo.
Some Savoury Snack Options for Diabetes
- Low-fat crackers such as Ryvita, real foods corn thins, or vita grains using 1 to 2 tablespoons of low-fat cottage cheese, or low-fat cheddar cheese
- Vegetables such as cucumber, carrot, capsicum sticks, or tomatoes with the dip of low-fat cottage cheese
- 3 cups of homemade popcorns
- 1 slice of multigrain toast with grilled mushrooms, and one teaspoon of low-fat grated cheese
- 1 cup of homemade vegetable soup
- Roasted chickpeas or fava beans
Though snacks are used to meet cravings often and act as a major part of our diet. So, a gestational diabetes diet should have all the healthy snack options to meet cravings and ensure better nutrition.
Foods that are Not Advised for a Diabetic Person
Simple Carbohydrates
Simple carbohydrate food sources have a very high glycemic index. They raise blood glucose levels fastly after eating. So, these simple carbohydrates, like pasta, noodles, potatoes, corn, and lentils, are not recommended for a diabetic person.
If a person is taking milk and yogurt, he should try to have them without added sugar.
Fatty Foods
If you’re gaining weight too quickly, start by reducing your intake of high-calorie foods. Foods that are high in fat include pastries, biscuits, and fried items. Cook with minimal oil and go for grilled, steamed, or baked foods rather than fried ones. Your dietitian can provide you with further advice and support if necessary.
Skipping these high-caloric foods and replacing them with healthy options proves the best choice for diabetes cure. So, avoid all this unhealthy stuff to get better gestational diabetes treatment.
One Day Meal Plan for a Woman Facing Gestational Diabetes
I am text block. Click edit button to change this text. Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
| MEAL TIME | MEAL OPTIONS |
| BREAKFAST
6-8am |
1 small bowl of cooked rice or 11/2 cup cooked oatmeal porridge |
| MID MORNING
9-10am |
1 handful of fruit or 1 glass skim milk/soy milk |
| LUNCH
12-1pm |
1 small bowl of cooked rice or 11/2 cup noodles+ 1 ounce lean meat |
| MID AFTERNOON
3-4pm |
1 handful of dry fruits/ one cup sugar free yogurt |
| DINNER
6-7pm |
1 large serve of vegetables _ 1 ounce fish |
| BEDTIME SNACK
9-10pm |
1 glass soy milk |
Set gestational diabetes diet in a healthy range to cure it effectively and minimize the risk of future complications.
Ensure a Healthy Future by Eating Healthy Today
After experiencing gestational diabetes, you are more likely to gain type 2 diabetes later. There is a higher chance that you will experience gestational diabetes if you become pregnant again.
Your chance of acquiring type 2 diabetes can be decreased by eating healthy and exercising regularly. Between one to three years, ensure to get type 2 diabetes screening. It should be based on your risk variables and the outcomes of your oral glucose tolerance test.
Gestational diabetes food selection is very critical. Along with the consumption of healthy foods, some lifestyle modifications are recommended. Here are some of those;
- Try to be in the healthy weight range
- Try to eat healthily and prefer nutritious food choices
- Engage yourself in proper physical activity every day
The incidence of type 2 diabetes and childhood obesity among children born to mothers who experience gestational diabetes is also higher. To lower this risk, it is advised for the entire family to practice healthy eating and regular exercise.
Lastly, ensure healthy living and decrease the risk of future complications by follow-up for type 2 diabetes checks.
Takeaway
Your chance of developing diabetes in the subsequent pregnancy and later in life rise if you have gestational diabetes. After giving birth, it’s critical to keep up your exercise routine, monitor your weight, and adhere to a healthy diet.
If you follow these tips, diabetes may not affect you as you age.
You Might Also Like
-
Raazi 5 Min
Why is it Crucial to Stop Smoking During Pregnancy When You Have Gestational Diabetes?
-
Raazi 5 Min
Whooping Cough and Pregnancy: What Expectant Mothers Need to Know
-
Raazi 7 Min
Weight Gain in Pregnancy Breakdown: What’s Normal and What’s Not
-
Raazi 6 Min
The Complete Guide to Morning Sickness
-
Raazi 6 Min
Supplements You Should Avoid During Pregnancy