When it comes to comparing osteoarthritis with rheumatoid arthritis, we come to know apparent lines of distinctions. Osteoarthritis and rheumatoid arthritis differ based on cause, symptoms, treatment, onset age, and speed. Before we discuss osteoarthritis vs rheumatoid arthritis, let’s first define both terms separately.
Rheumatoid arthritis is a disorder that develops whenever the immune system within the body erroneously assaults healthy cells, which leads to the emergence of the sickness. This disease produces considerable inflammation (swelling) in the joints, which may eventually result in joint deformity if left untreated. The rheumatoid arthritis symptoms most often manifest themselves in the joints, and the condition strikes a cluster or group of joints all at once.
Osteoarthritis handles most occurrences of arthritis. This condition may be thought of as a kind of joint retrogression. The hands, hips, and knees are the most prevalent places where this illness manifests itself. When a person gets osteoarthritis, the cartilage in their joints disintegrates, and the bone seen below begins to change.
- Rheumatoid arthritis can cause deformities like ulnar drift and swan neck.
- Osteoarthritis affects weight-bearing joints due to cartilage wear.
- Rheumatoid arthritis involves systemic symptoms like fatigue and fever.
- Morning stiffness lasts over an hour in rheumatoid arthritis.
- Rheumatoid arthritis can affect organs like the lungs and heart.
- Osteoarthritis progression is unpredictable and can be severe.
- Rheumatoid arthritis is more common in women, osteoarthritis increases with age.
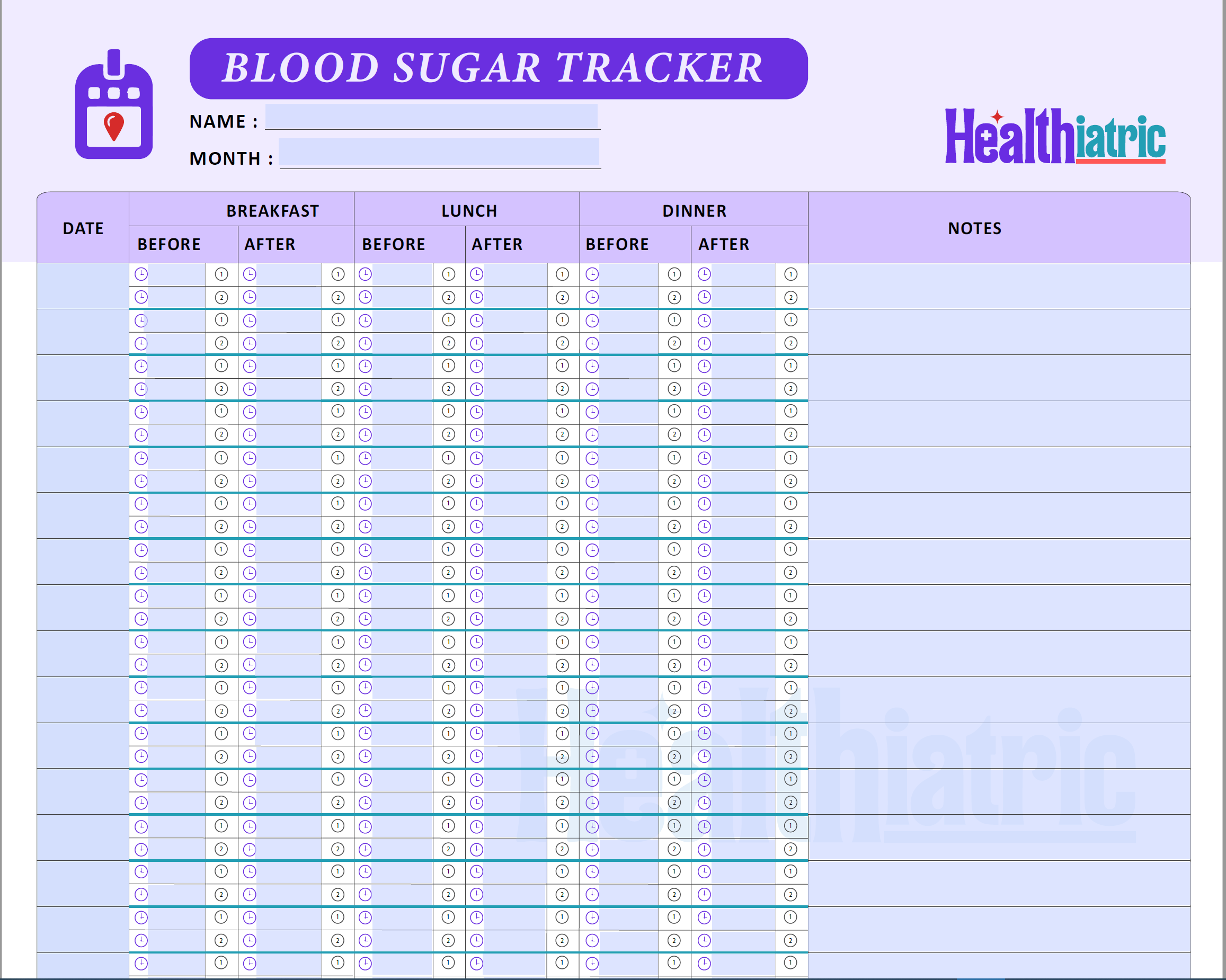
How Can You Differentiate Rheumatoid Arthritis from Osteoarthritis?
| Characteristics | Rheumatoid Arthritis | Osteoarthritis | |
| 1 | Symptoms | Aching joints
Swollen tissue Inflammation lumps or nodules |
Stiffness
Prone to fractures Dull yellow, granular, and soft cartilage Wear and tear with heavy use |
| 2 | Cause | Autoimmune | Age |
| 3 | Onset Age | Any age, mostly 30-50 | Later years |
| 4 | Morning stiffness | More than one hour | Less than one hour |
| 5 | Effects whole body or not | Effects joints and other organs | Only affects joints |
| 6 | Risk factors | Heredity
Environmental pollutants Infections |
Being older
Cartilage destruction due to constant use Estrogen reduction at menopause Obesity Increased stress on joints Injury Frequent kneeling and stooping |
| 7 | Symmetrical or Asymmetrical | Symmetrical | Asymmetrical |
| 8 | Speed of onset | Few weeks to a few months | Unpredictable |
| 9 | Require surgery or not | Not a viable option | Joint arthroplasty |
| 10 | Joint deformity | Ulnar drift
Boutonniere deformity Hallux Swan’s neck deformity |
Crooked or deformed joints as the disease advances |
What are the Symptoms of Osteoarthritis and Rheumatoid Arthritis?
Osteoarthritis and rheumatoid arthritis may cause similar symptoms, but distinguishing between the two is crucial for selecting the appropriate therapy.
Rheumatoid arthritis symptoms include
- Achy muscles as well as organs that have increased in size.
- Joints of hands, feet, wrists, elbows, knees, and ankles are especially susceptible to injury.
- The damage to joints caused by inflammation might be irreparable if not treated.
- A bodily evident disease; lumps or nodules. These may also develop on the knuckles and the areas surrounding the elbows.
Osteoarthritis symptoms include
In Osteoarthritis, the patient feels pain and tenderness in the joints but usually experiences minor swelling. The symptoms of osteoarthritis involve
- The stiffness comes after prolonged intervals of stillness and slumber. Its duration lasts for the first 30 minutes.
- Being prone to fractures
- The color of the cartilage changes to a pale yellow, as well as becoming granular, mushy, and less flexible.
- Cartilage is less able to resist wear and tear with heavy use.
Causes of Rheumatoid Arthritis and Osteoarthritis
Rheumatoid arthritis is an autoimmune disease, while the cause of rheumatoid arthritis is constant wear and tear and direct damage or instability. Joint inflammation, stiffness, and soreness are all indications of this disorder, which arises when your immune system, which would typically combat infection, attacks the cells that line your joints instead. This condition is known as inflammatory arthritis. Consequently, the cartilage and bone surrounding the joints may degrade over time.
Causes of osteoarthritis are that OA develops whenever cartilage and other joint tissues deteriorate or undergo a structural change. However, simply degeneration of the joints is not the source of this problem. Instead, the deterioration may be triggered by tissue changes, often occurring slowly over time.
Onset Age for Rheumatoid Arthritis and Osteoarthritis
Rheumatoid arthritis symptoms might appear at any point in a person’s life. This disease may strike at any age, although it most often appears in middle age, making it a disease of the ancestors. If someone in your lineage has rheumatoid arthritis, there is a greater chance that you may also get the condition at some point in your life.
However, osteoarthritis often manifests in one’s later years.
Osteoarthritis and Rheumatoid Arthritis Morning Sickness
For rheumatoid arthritis, having morning stiffness linger more than an hour is expected. Morning soreness often subsides during the first hour of the day. After being active, or at the end of the day, stiffness returns. The symptoms include chronic tiredness and overall malaise. There are no systemic signs.
For Osteoarthritis, the duration of morning stiffness is often under one hour. There is a recurrence of stiffness at the day’s conclusion or after prolonged use. There is a sound that may be described as grating, grinding, or cracking whenever the joint is moved. Morning stiffness is a common term that refers to the discomfort and stiffness people experience upon waking up in the morning. OA-related stiffness often disappears within 30 minutes. If the joint is inflamed, the pain may last for longer than 30 minutes.
Arthritis that Affects the Whole Body
Rheumatoid arthritis affects the whole body. It evidences extreme weariness and a pervasive sense of illness. Inflammation is a hallmark of rheumatoid arthritis, a chronic autoimmune condition that may have far-reaching effects beyond the joints. The skin, eyes, lungs, heart, and blood vessels are just some organs that the illness might negatively impact.
Knee and finger arthritis may cause unbearable pain and swelling. However, the skin, the eyes, and the lungs are all vulnerable. Rheumatoid arthritis (RA) is indeed a systemic disorder, which means that it may express itself in a variety of ways across the body. However, osteoarthritis does not show any systemic signs.
The disabling consequences of osteoarthritis are more likely to manifest in the hands, lower back, neck, and weight-bearing joints (knees, hips, and feet). Osteoarthritis only hurts the joints of a person’s body.
RA VS. OA- What Are The Risk Factors For Arthritis?
It seems that the risk of rheumatoid arthritis is increased by heredity, environmental pollutants, infections, and hormones. It is more likely that a person will get RA if a close family (such as a parent, sibling, or other relatives) already has the illness. Environmental factors like smoking and alcohol use are examples of behaviors that contribute to an increased risk. In addition, rheumatoid arthritis and many drugs used to treat it have been shown to have an immunosuppressive effect, which may increase the risk of infection.
However, for Osteoarthritis, the risk factors are being older, cartilage destruction because of constant use, estrogen reduction at menopause, obesity, increased joint stress, injury, frequent kneeling, and stooping. Cartilage osteoarthritic can destroy as early as 20, and feeling signs at 40.
Is Osteoarthritis Or Rheumatoid Arthritis Symmetrical?
When understanding osteoarthritis vs rheumatoid arthritis symptoms of both play a very important role. While symptoms of symmetric arthritis affect the same joints on both sides of the body, those of asymmetric arthritis are limited to one side.
Joint involvement is symmetric in rheumatoid arthritis. It usually manifests in symmetrical locations, including hands, wrists, or elbows, both balls of the feet, and so forth. Regarding detecting an autoimmune illness, symmetry is the most crucial factor. However, a person can experience symptoms on just one side of their body when the sickness manifests. The condition will ultimately reach a state of symmetry if it is allowed to continue to expand. It is fairly rare for symptoms of osteoarthritis to first appear on one side of a person’s body before spreading to the other, despite the fact that the condition is asymmetric.
Joints that are closest to the fingernails or thumbs, large fat mass joints (hips, knees), or the spine are often the first to display symptoms, and their progression is typically slow and steady. Although Osteoarthritis might asymmetrically present itself, the condition often affects both joints as time passes.
Which One Excels In the Speed of Starting The Disease: Rheumatoid Arthritis or Osteoarthritis?
In most situations, the symptoms of rheumatoid arthritis appear gradually throughout some weeks; however, the condition may sometimes worsen rapidly over a few days. The symptoms might differ from one person to another in succession. They could come and go or change with time. When your health worsens and your symptoms grow more severe, you may have episodes of inflammation known as flares.
Rheumatoid arthritis starts quickly, lasting from a few weeks to a few months. The additional strain that being overweight places on your joints, which may hasten the breakdown of cartilage in your joints, makes Obesity one of the most significant risk factors for Osteoarthritis.
People who have a BMI of 30 or above or who are obese have a higher risk of developing osteoarthritis. The progression of osteoarthritis cannot be accurately predicted and does not adhere to a set pattern. Even if the joint seems to be in a severe state on the X-ray, the condition can go unnoticed for an extended period and not present itself. However, it is also possible for the need to quickly deteriorate for many weeks or months even while the X-rays seem normal. Oa starts gradually, for several years.
Which Type of Arthritis Requires Surgery?
In the case of rheumatoid arthritis, surgery is not a viable therapy option. Therefore, most individuals with rheumatoid arthritis never have surgery, although, similar to those with Osteoarthritis, people with rheumatoid arthritis may choose to undergo surgery to relieve joint discomfort and enhance their ability to function in day-to-day life. Joint replacement, arthrodesis, and synovectomy are the three operations that are performed the most often.
Rheumatoid arthritis may require surgery known as arthrodesis or fusion for someone with significant joint deterioration due to osteoarthritis or inflammatory arthritis. The bone fragments that have recently resected will be fused back together by the surgeon with the use of metal pins, plates, or rods during this process.
While in the case of Osteoarthritis, Replacement surgery/ ORIF surgery (arthroplasty) cannot be fixed otherwise. Conservative surgery, in which the patient’s damaged cartilage is left in situ; radical surgery, in which the patient’s cartilage is replaced with an artificial endoprosthesis; both surgical procedures are referred to as joint arthroplasty.
What Are The Deformities of Rheumatoid Arthritis and Osteoarthritis?
In rheumatoid arthritis, it occurs in connective tissue – synovial joints. Mostly small joints like fingers. It has a needle-spindle-shaped appearance. The joint becomes tender, painful, and warm due to inflammation. Typical deformities are:
- Ulnar drift
- Boutonniere deformity
- Hallux
- Swan’s neck deformity
The changes in osteoarthritis typically develop slowly over several years. However, there are some outliers. Inflammation, as well as an injury, is the most prevalent cause of bony alterations, the degeneration of muscles and ligaments, and the destruction of cartilage, all of which may manifest in joint deformity, discomfort, and edema. In addition, joints affected by osteoarthritis may become crooked or deformed as the disease advances.
Takeaway
Although Rheumatoid arthritis and Osteoarthritis are similar in many respects, the ten above features differentiate them more easily. . When you are familiar with these characteristics and have a good understanding of them, it will be much simpler for you to differentiate between the two. As our comparison of osteoarthritis vs rheumatoid arthritis came to a close, we discovered that rheumatoid arthritis is an autoimmune disease that leads to swelling of the joints. It is also possible for it to influence other parts of the body. It is a chronic condition that can worsen over time and affect the ability to work, exercise, and do everyday activities.
On the other hand, osteoarthritis is a degenerative condition affecting weight-bearing joints such as knees and hips. It’s caused by wear-and-tear cartilage in the joint. With this information, you can also differentiate your arthritis issues and take early precautions to avoid any form of arthritis.
You Might Also Like
-
heena256 9 Min
Arthritis in Children: Unveiling the Impact and Challenges of this Condition
-
admin 7.30 Min
The importance of Exercise To Reduce Obesity and Joint Pain
-
admin 7.30 Min
Seven Most Effective Supplements for Healthy Joints
-
admin 30 Min
Rheumatoid Arthritis: Symptoms, Diagnosis, and Treatment
-
admin 25 Min
Osteoarthritis: Symptoms, Diagnosis and Treatment